OPED: New hope for people with HIV
A new study holds promise for people living with HIV who have limited therapy options or rely on complex drug regimens
A new international study led by a researcher from New York-Presbyterian Queens, published in The New England Journal of Medicine on May 11, demonstrated the effectiveness of an investigational long-acting, first-in-class therapy for people with multi-drug resistant HIV – signaling the potential for a radically simplified drug treatment and improved compliance among patients living with HIV.
In the randomized controlled, double-blind trial known as “CAPELLA,” injections beneath the skin of an investigational HIV agent called lenacapavir significantly suppressed the viral level in patients with HIV who were currently on a failing antiretroviral treatment regimen. Importantly, viral suppression remained high for six months.
If approved, the new therapy has the potential to be a game-changer in several ways, according to the study’s lead author, Dr. Sorana Segal-Maurer, director of the Dr. James J. Rahal, Jr. Division of Infectious Diseases at NewYork-Presbyterian Queens and a professor of clinical medicine at Weill Cornell Medicine.
“The encouraging results of the study offer hope for people living with HIV who have limited therapy options, as well as those who are reliant on complex drug regimens,” Dr. Segal-Maurer said. “Lenacapavir has the potential to be used as either a long-acting pill or a subcutaneous injection every six months, which anyone can be taught to do. I cannot even find the words to share what that means to all our patients, but especially those with limited or no treatment options, or whose unique circumstances make it difficult to engage in care.”
However, she stressed, that patients still need to be highly adherent to the rest of their antiretroviral medications that make up their complete regimen.
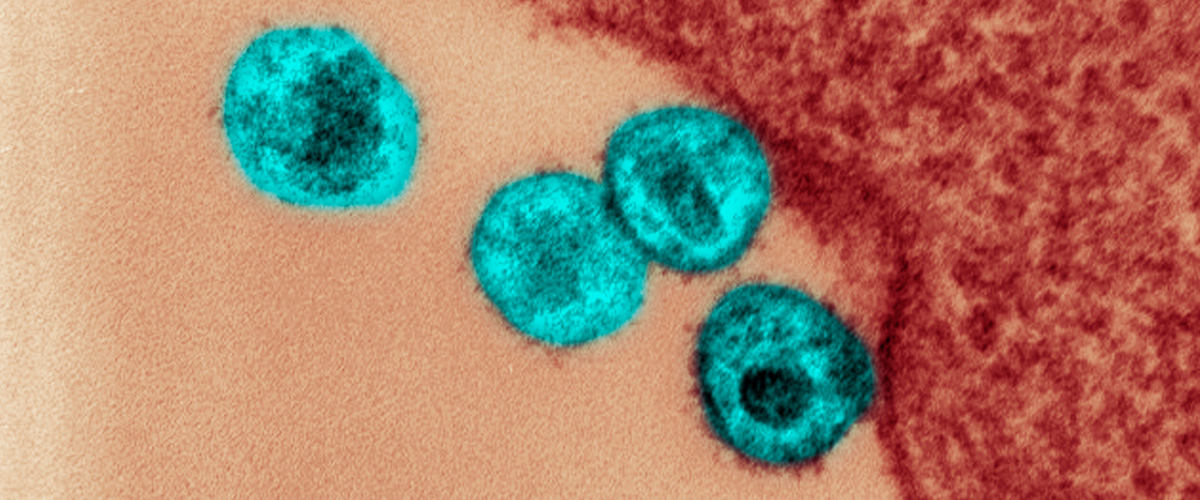
Lenacapavir, from Gilead Sciences, is an investigational antiretroviral medicine called a capsid inhibitor that targets the cone-shaped shell of the virus and proteins important to viral reproduction. Previous research showed that lenacapavir interrupts multiple stages in the viral life cycle, helping to suppress the virus.
New York-Presbyterian Queens was one of 42 investigational sites for lenacapavir around the world.
“Despite significant advances in antiretroviral treatments that have helped many people with HIV suppress the virus, there are still patients with treatment failures due to viral resistance or unacceptable side effects,” Segal-Maurer added. “These patients no longer have viral suppression and require treatment options that can be complex and difficult to adhere to, leading to further drug resistance. These challenges underscore the importance of new treatment options for people living with multi-drug resistant HIV infection.”
The phase II/III CAPELLA trial included 72 people living with HIV with a median age of 52, 75 percent of whom were men. Individuals were eligible for the study if they were age 12 and older, were currently on a failing drug regimen, and had developed resistance to at least two drugs from four main classes of antiretroviral medications (46 percent of patients in the study had resistance to all four major classes of antiretroviral medications). Half of the trial participants were randomized to receive oral lenacapavir or a placebo along with their existing medication regimen for 14 days.
The remaining 36 participants started taking lenacapavir pills at the beginning of the trial on top of a regimen of HIV medications designed to maximize effectiveness for these heavily treatment-experienced people. After 14 days on the oral drug, they, too, switched to the subcutaneous injections.
At the end of the lead-in period, 88 percent of participants receiving lenacapavir saw a significant drop in their viral level, compared with just 17 percent of those on the placebo. Trial participants randomized to receive lenacapavir also experienced an increase in white blood cells called CD4 T cells, critical to fighting the infection. Overall, the percentage of people with profoundly low CD4 T cells decreased from 24 percent to 0 percent. No one dropped out of the study as a result of drug-related side effects, according to Dr. Segal-Maurer.
“The significance of the trial’s findings is profound. We’ve come a long way,” said Segal-Maurer, who has witnessed the evolution of HIV treatment over the decades, starting at the beginning of the AIDS epidemic. “I was in medical school in the early to mid-eighties when the average lifespan between diagnosis and death was anywhere from weeks to months. We’ve gone from many pills multiple times a day to one pill a day to possibly even less. Now we’re in a place where if a patient can engage in care and take their medicine, they have an excellent chance for improved outcomes and a long lifespan.”
A version of this op-ed can be found on the New York-Presbyterian Queens “Health Matters” website.
Dr. Sorana Segal-Maurer is a paid consultant for Gilead Sciences and director of Dr. James J. Rahal, Jr., Infectious Diseases Division at New York-Presbyterian Queens, and professor of clinical medicine at Weill Cornell Medicine. She is the site principal investigator for a number of studies evaluating new investigational HIV antiretroviral therapies.